As winter arrives and skiing enthusiasts eagerly take to the slopes, the risk of thumb injuries, notably Skier's Thumb, increases significantly. This specific injury comprises 5-10% of all skiing-related injuries and is notably the most common upper extremity injury among skiers. Understanding the anatomy and mechanics behind Skier's Thumb is essential for diagnosis and management.
The Anatomy Behind the Injury
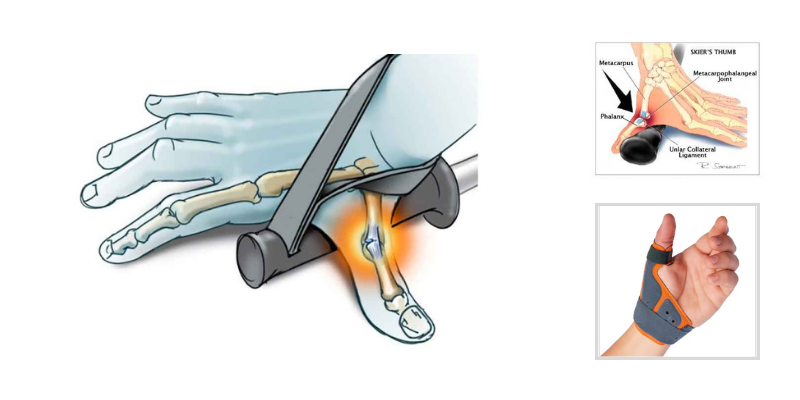
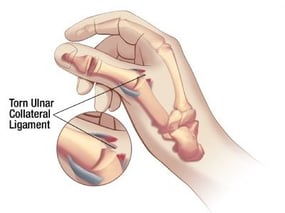
Understanding the anatomy of the thumb is crucial to comprehending how certain injuries occur, especially those affecting the metacarpal phalangeal (MP) joint, the second joint of the thumb. A key player in the stability of this joint is the ulnar collateral ligament (UCL). This ligament acts as a primary stabilizer, originating at the distal portion of the thumb metacarpal bone on the ulnar or index side and inserting on the inside of the proximal phalanx bone, crossing over the MP joint. Its primary function is to provide stability against radially directed or valgus forces, such as those pushing the thumb from the index side.
Skiers Thumb:
Skier’s Thumb Defined
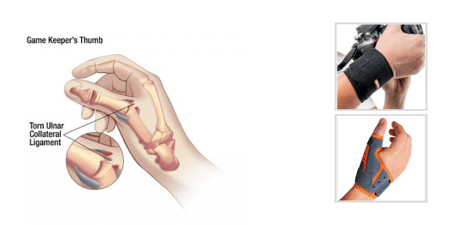
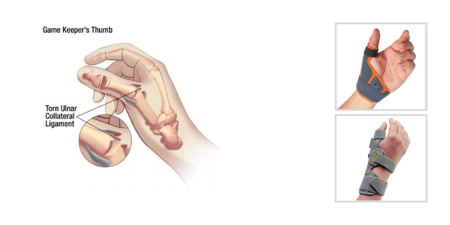
The term "Skier’s thumb" is often used to describe an acute injury to the UCL, setting it apart from "Gamekeeper’s thumb," which results from repetitive stress to the ligament. Despite the similarity in the tearing or rupture of the UCL, the mechanism of injury is what differentiates the two conditions. Skier’s thumb typically occurs when a skier falls on an open or abducted thumb or when a ski pole is forcibly removed from the hand, causing sudden trauma to the UCL of the thumb MP joint.
The spectrum of UCL injuries ranges from partial tearing of some fibers to a complete rupture of the entire ligament. Such injuries usually manifest as swelling and pain at the MP joint. In cases of complete rupture, there may even be a visible deformity, where the proximal phalanx deviates radially due to the compromised support at the ulnar aspect of the joint.
Finding and Treating Skier’s Thumb
If a UCL injury is suspected, the first step is to palpate the ligament to check for tenderness. Applying gentle valgus stress—by pulling the proximal phalanx of the thumb away from the hand—can further assess the injury. This should be done while supporting the thumb metacarpal, both with the metacarpophalangeal (MP) joint in full extension and at approximately 30 degrees of flexion. Pain during palpation or when stress is applied may indicate skier's thumb. An increase in motion during valgus testing can also signal injury, but it's important to compare with the non-injured thumb to establish a baseline for joint laxity.
A complete rupture of the UCL, characterized by more than 15 degrees of laxity when stress is applied to the joint, typically requires surgical intervention. A hand surgeon can perform a repair to restore the ligament's function. On the other hand, a partial tear or sprain, where there's pain during stress or palpation but no obvious laxity, often benefits from conservative management. Immobilization with an orthosis can provide the necessary support to the MP joint, preventing any stress on the UCL while the fibers heal. It's recommended to use an orthosis for 4-6 weeks, gradually reducing its use based on symptoms.
During the acute phase of injury, a splint like the Fix Comfort Thumb Brace can immobilize the MP joint, providing the necessary support for healing.
As the acute phase subsides, a protective orthosis such as the Thumsaver MP is recommended to offer the stability needed to return to activities while protecting the UCL ligament fibers for long term healing without limiting function or motion at the thumb unnecessarily.
Blog References: For more information on this topic, click to see the references for this blog post