Osteoarthritis (OA), or the degeneration of a joint, commonly occurs at the base of the thumb. OA at this joint is diagnosed with conventional radiographs (x-rays), but often can be recognized based on symptoms. Symptoms occur predominantly with pain at the base of the thumb, especially when performing tasks that require a pinch (i.e. pulling on socks). This disease progression can occur with a thumb deformity, but may be symptomatic without an obvious change in the thumbs appearance.
What causes the thumb deformity?
Wear and tear of the bones, and of the ligaments and muscles that surround the base joint (TMC, also called the CMC) of the thumb occurs commonly during tasks that require a resisted pinch or grip. Ligaments that normally provide joint support can become weak and lax and less able to absorb forces thereby contributing to degeneration at this joint.
What is the deformity?
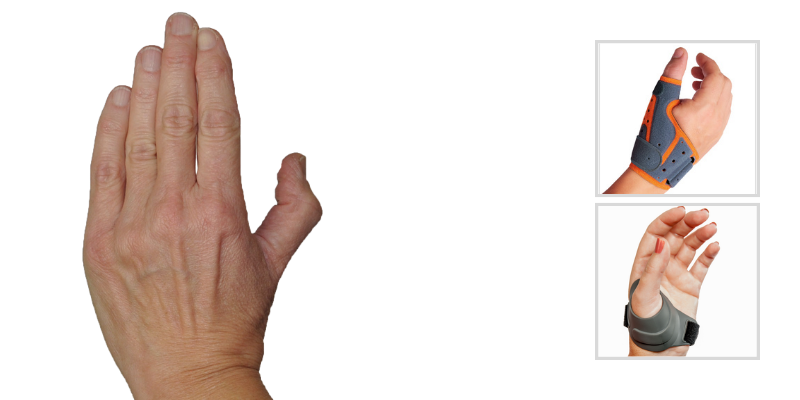
Several deformities are possible with OA at the base of the thumb, but one particular deformity pattern (the Zig Zag deformity) is most common. With weakening of the stabilizing ligaments, the joint has a tendency to become flexed and adducted meaning the thumb moves closer into the palm of the hand. Over time, the small thumb muscles can tighten causing closure of the first web space making it difficult to move the thumb away from the palm. As this posture becomes fixed, the metacarpal phalangeal (MP) joint of the thumb compensates by overstretching into hyperextension. Eventually the interphalangeal (IP) joint may move into a flexed posture related to the change in pull of the soft tissue and tendons.
How do I assess what thumb orthosis to fabricate or recommend?
The key factors to consider when assessing orthotic intervention for a zigzag deformity are, how to counteract the deforming forces and how to position the thumb for function.
- The first step in examining the thumb to determine what orthotic intervention, if any, works best, is to manually position the TMC in abduction and resist adduction as your patient attempts to oppose the index finger. This maneuver and the patients response will tell you if an orthosis that holds this posture will be helpful and desirable to the patient.
- If MPJ hyperextension persists once the TMC is stabilized in abduction, manually block the MP joint in neutral to slight flexion to assess if this provides further control and strength when your patient attempts a lateral pinch. If the answer is yes, then your orthosis should mimic this position.
- Whether you are custom fabricating an orthosis or adapting a prefabricated one, it is important to assess if the design will provide the required stabilization and position to restore the thumb’s architecture and provide your patient function and pain relief.
There a variety of options to assist with providing comfort and increased function for individuals with OA at the base of the thumb including the 3pp ThumSling, the Fix Comfort Thumb Brace, and CMCcare Thumb Brace.

|
 |

|
| 3pp ThumSling | Fix Comfort Thumb Brace | CMCcare Thumb Brace |
There doesn't have to be deformity for an orthosis to be beneficial. Symptoms will dictate the appropriateness of orthotic intervention. In advanced arthritis with fixed deformities, orthotic intervention may not be the appropriate choice and the patient should be referred to a hand surgeon for further evaluation.
Blog References: For more information on this topic, click to see the references for this blog post