What Is a Mallet Finger?
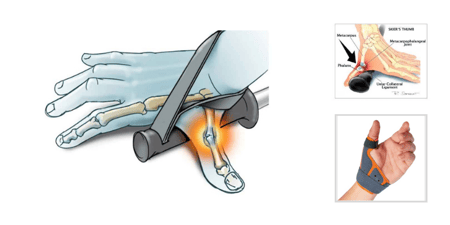
From professional athletes to homemakers, mallet finger, also known as “baseball finger” is a common injury of the finger. A mallet finger injury often occurs from a direct trauma to the tip of an extended finger which causes a disruption of the tendon responsible for extending the distal phalangeal joint (DIPJ). A mallet finger can occur with or without a fracture or bony avulsion
Doyle’s classification system for Mallet Finger Injuries describes levels of severity from Type I; a closed injury without an avulsion fracture, Type II; open laceration without fracture, to Type IV fractures with involvement of the articular surface. Determining the severity of the injury is important to determine the appropriate treatment regime.
The most common Type I and Type II injuries, caused by high velocity sport injuries and household and work related activities, are not an inconsequential injury. It has been reported that mallet finger can cause a loss of work for up to 6 weeks. Adverse side effects include residual extensor lag, a dorsal bump, or a swan-neck deformity.
Treatment for Type I or Type II Mallet Finger
The choice of conservative treatment for Type I and Type II injuries is with orthotic/splinting intervention. While there is agreement on use of an orthosis for mallet finger, there is some disagreement on splint preference, duration of full-time wear and the need for supplemental nighttime wear.
In studies examining custom splints versus pre-fabricated splints such as the Oval-8 Finger Splint for a mallet injury, the general consensus is that either option results in similar outcomes. What is important is recommending a splint that is durable enough to hold up to everyday use and is easily managed by the patient.
Time Recommendations
Early treatment is preferable but even delayed treatment can be successful with good patient compliance with full time splinting. The time recommended for splint wear varies from 5-12 weeks, with a minimum of six (6) weeks the most common duration. Eight (8) weeks should be considered for chronic mallet injuries.
Following the initial 6 weeks of full time wear, night wear may be recommended. There is evidence that recommending continued night wear for approximately 2 weeks may be effective especially if the injury is chronic or an extensor lag persists. Presenting this option to the patient as a nighttime “retainer” similar to that used in orthodonture, makes it easy to explain the advantages of splinting during periods of rest.
Patient Considerations
Patient preference, satisfaction and compliance are important considerations when choosing a splint. The following provides a synopsis of treatment considerations;
- The splint should be strong enough to withstand everyday use.
- The splint should be satisfactory to your patient, be easy to manage independently and should be comfortable to facilitate compliance.
- Patients must understand that full time wear of the splint is not optional
- Patients should be educated to monitor skin condition, circulation and changes in finger size that affect how the orthosis fits
- The initial immobilization period should be 6 weeks (acute) – 8 weeks (chronic).
- A recommendation to continue an additional 2 or more weeks of night wear.
There are many splints to choose from, including closed design plastic splints and aluminum and foam splints that cover the volar surface of the distal phalanx, to the open design. Oval-8 Finger Splints (available in Classic beige and NEW Oval-8 CLEAR) that leaves the pad of the fingertip free for function.
Follow up visits should be scheduled during the 6-8 week treatment time to monitor skin condition and to adjust the fit of the splint. Several visits may be necessary once the splint is removed to instruct the patient in progressive range of motion exercises and strengthening if needed.
For a comparison of prefabricated splint options, please read our blog-Splinting Options for Treating a Mallet Finger.
Blog References: For more information on this topic, click to see the references for this blog post