Causes of Deformity in the Rheumatoid Thumb
Rheumatoid arthritis (RA) is a destructive inflammatory disease that impacts soft tissue. This disease commonly involves the thumb and causes deformities to the thumb through tendon rupture or tendon subluxation and the abnormal stretching of ligaments and other joint structures.
There are 6 Different Identified Deformities for the Rheumatoid Thumb:
Type I Thumb Deformity (Boutonniere)
- The most common identified type, it has been reported that 50% to 74% of patients with finger deformity due to RA are Type I deformities
- Metacarpal phalangeal (MP) joint flexion and interphalangeal (IP) joint hyperextension
- This “Z” posture classically develops from synovitis at the MP joint that stretches the extensor mechanism
Type II Thumb Deformity
- This uncommon presentation is similar to type I with MP flexion and IP hyperextension but also involves and originates with adduction at the trapeziometacarpal (TMC) joint
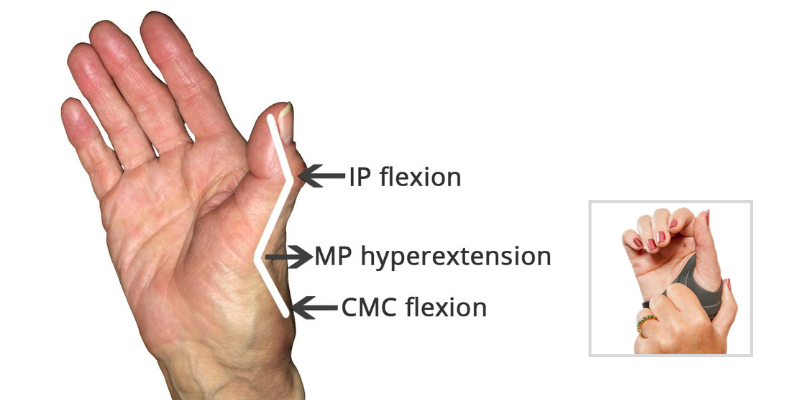
Type III Thumb Deformity (Swan Neck)
- Also originates at the TMC joint and occurs with TMC adduction, but involves MP hyperextension and IP flexion
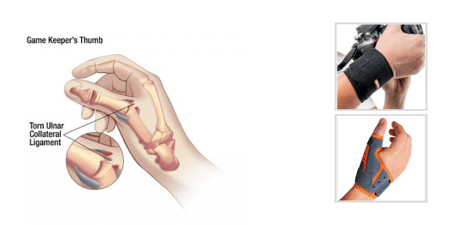
Type IV Thumb Deformity (Gamekeeper's)
- Usually occurs with laxity of the ulnar collateral ligament at the thumb MP joint related to synovitis
- Typically, the proximal phalanx of the thumb deviates laterally and then the TMC joint goes into adduction
Type V Thumb Deformity
- Soft tissue at the volar MP joint stretches causing MP hyperextension
- IP may then become flexed, but the TMC joint is not usually involved
Type VI Thumb Deformity (Arthritis Mutilans)
- Characterized by loss of bone substance
- Is specific to individuals with arthritis mutilans
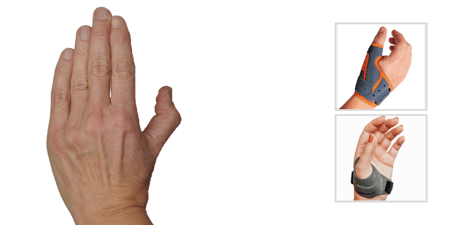
Assessing Which Thumb Orthosis to Fabricate/Recommend
Using an orthosis is typically recommended for the rheumatoid thumb when the deformities are passively correctable and is thought to be more effective with milder cases of the disease. An orthosis for the rheumatoid thumb should assist with balancing soft tissue forces and placing the joints in an appropriate or more neutral position. In other words, it is recommended that a therapist provide support to the deformed thumb using their hands in order to determine which joint(s) can be supported to allow the thumb a more normal mechanical pattern.
Typically it is helpful to first try supporting the joint initiating the deformity. For example, for a type IV deformity, apply support to the MP joint to determine if a corrected position at this joint allows function without pain and allows good mechanics. Continue adding support to the joints as needed. Once the joints to be included in the orthosis are determined, find or fabricate an option that provides the needed support.
Orthoses have been found to be effective in decreasing pain when worn during the day for individuals with a rheumatoid thumb and the orthosis was not found to disrupt grip, pinch, function, or dexterity. Studies suggest that individuals with RA have decreased pain when using an orthosis during sleep and may prefer a soft splint instead of a harder design.
| CMCcare Thumb Brace | 3pp EZ Fit Thumb Spica Splint | ThumSaver MP |
 |
 |
 |
| Thumb Arthritis | de Quervain's | Gamekeeper's Thumb |
For more information on orthoses for RA thumb deformities, take a look at our complete line of Thumb Orthoses.
Blog References: For more information on this topic, click to see the references for this blog post