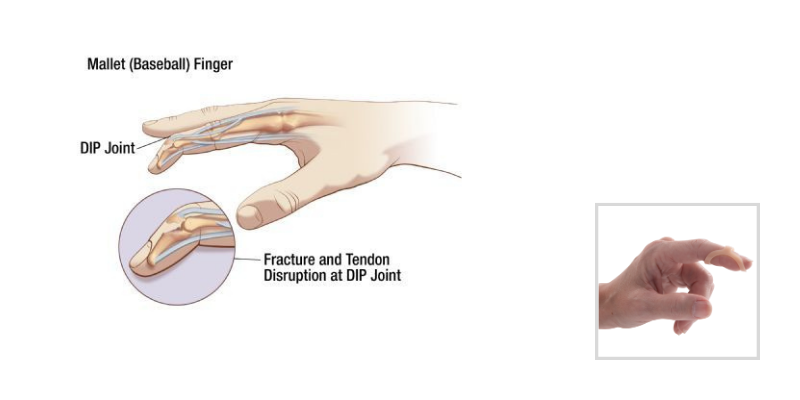
If you ask 10 different hand therapist how they treat mallet finger injuries, you may just get 10 variations on an answer that is ultimately some form of immobilization of the involved distal interphalangeal (DIP) joint. Systematic review of the studies on conservatively treated mallet finger injuries is not able to identify which orthosis is most optimal and what the most appropriate wear time is, and therefore recommends that the orthotic material choice should be based on the treatment provider’s comfort and the patient’s lifestyle and concerns.
This same analysis of the research suggests use of the orthosis for 6 weeks for acute mallet injuries and 8 weeks for chronic injuries with possible use at night during sleep following the initial immobilization period. So basically, the research evidence currently leaves room for hand therapists and surgeons to use their clinical experience in treating these injuries. However, what the research does tell us is that individuals with mallet finger injuries who are compliant have significantly better outcomes than those individuals who are not compliant. Browsing through the Journal of Hand Therapy allows us to find the presentation of several ideas for treatment of mallet finger injuries that keep this finding in mind. The ideas for immobilization technique discussed in the journal include casting, percutaneous pinning, and taping.
Clinical Protocol
One orthopaedic practice that is highly supportive of offering client centered treatment is currently using a protocol for simple boney and tendinous mallet injuries which includes six weeks of Kinesiotaping and Oval-8 Finger Splints orthosis use.
The tape is applied from volar to dorsal in a fashion that pulls and holds the DIP in extension. Over the top and to ensure full extension of the involved DIP, the appropriate oval 8 orthosis is applied with a little more tape applied to the orthosis to ensure it stays in place. Patients are seen weekly for 6 weeks to change the tape and for a quick clinical check. Following the initial 6 weeks of immobilization, the orthosis may be continued if there is an extension lag or may just be continued during risky activities (i.e. sports) or at night during sleep for a few weeks. Individuals do not typically require any additional skilled therapy for this injury.
Why we like this current clinical protocol?
The above described protocol is not financially demanding and allows the patient to get his or her finger wet without interruption of the treatment and without damage/maceration of the skin on the involved digit. We believe compliance is increased because the immobilization does not need to be removed, but also does not interfere with hygiene and is said to be comfortable by those following the protocol. If the oval 8 begins to loosen, a heat gun can be used to easily adjust the fit. We are in need of research evidence on the use of this clinical protocol, but we see good results and our patients express satisfaction.
Click here for more information on Oval-8 Finger Splints